Can we delay Alzheimer’s progression?
Alzheimer’s disease (AD) is the most prevalent neurodegenerative disorder and primarily affects the learning and memory of an individual. A slow but gradual memory loss results in impairment of cognitive functions, which ultimately causes psychosis and dementia. AD is believed to be initiated as a result of protein aggregation, mainly by extracellular amyloid beta (Aβ) and intracellular Tau. Another aspect is the inefficient clearance of these protein aggregates from the central nervous system.
Microglia | The natural clearance system of the brain
In AD, the transformation of Aβ monomer into the soluble oligomers is considered a major event that causes actual damage to the nervous system. These soluble oligomers later transformed into a large number of insoluble fibrils and finally become plaques. Since long, microglia have been explored mostly for their neuro-inflammatory functions. However, the trend is now shifting towards their less explored functions that involve non-autonomous clearance of protein aggregates.
Whether microglia could be beneficial or detrimental to the brain, it all depends upon the type and strength of stimulus they received. It has been observed that with aging, microglia show a decline in their phagocytic behavior and could be responsible for Aβ accumulation in AD brains. But the question remains, why microglia lose their phagocytic activity in Alzheimer’s? Increasing evidence have led to an assumption that microglia could efficiently clear the Aβ and damaged neurons during the early stages of AD. However, as the disease progressed the protein aggregates clearance might be diminished due to reduced expression of several receptors as well as enzymes involved in phagocytosis and degradation of Aβ.
Microglial reprogramming
If the beneficial properties of microglia could be selectively harnessed without activating their pro-inflammatory response, a potential therapeutic strategy could be developed to check the formation of protein aggregates. To achieve this, several ways have been proposed which bank on treatment with microRNAs, cytokines, pharmacological agents, as well on nutrients supplementation. The protein aggregation usually begins in the brain silently much before any signs or symptoms are diagnosed in the patients. The major limitation in formulating any strategy against AD is to decide when we should start the treatment. Therefore, preventing or slowing down the speed of protein aggregation is more practical rather than preventing the damage caused by these aggregates.
Now the question arises, how to limit this protein aggregation and simultaneously clear whatever aggregates formed inside the brain? Although microglia efficiently take care of this in the adult brain, they lose this property in the aged AD brains. As mentioned earlier, if their phagocytic activity could be regulated then the rate of protein aggregation could also be checked. Recently, various plant derived compounds have been successfully explored as microglial modulators. The major benefit of these compounds is that they can be easily incorporated in our regular diet without any side effects, something which is missing from the existing marketed drugs for AD.
Sulforaphane | The microglia reprogrammer?

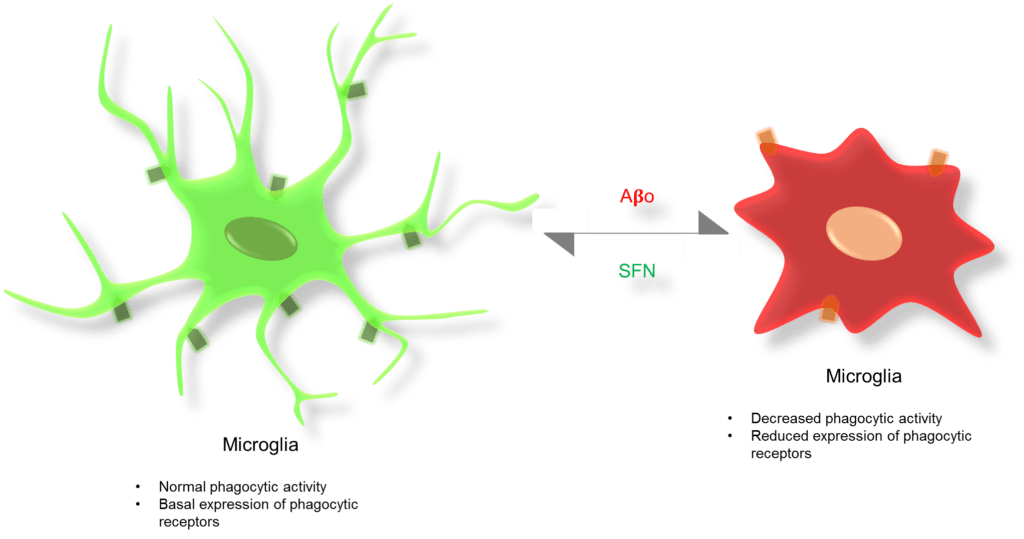
A recently explored compound is Sulforaphane (SFN), an isothiocyanate, which is present in the cruciferous vegetables like cabbage, brussel sprouts, cauliflower, and mostly in broccoli sprouts. SFN has shown to activate Nrf2 mediated antioxidant response pathway and also induce macrophages phagocytic activity. These properties make SFN as an attractive candidate to modulate microglia. Recently, our group has shown that SFN administration could prevent microglial phenotype switching when exposed with toxic amyloid oligomers. In addition, SFN treated microglia has shown a slight increase in their phagocytic activity and thereby successfully engulfed the Aβ oligomers in vitro. Previously, we have shown that SFN could improve the learning and memory of rodents if administered during their postnatal brain development. Taken together, our findings along with other reports have indicated that the inclusion of SFN in the diet may increase the chance of slowing down the progression of Alzheimer’s and other proteinopathies. Currently, we are involved in the further tweaking of SFN mediated microglial phenotype switching and trying to enhance their Aβ clearance function without activating the pro-inflammatory response in the aged rodent AD model.
Take home message: Add broccoli sprouts and other cruciferous vegetables in your diet.
Important Links
More about Alzheimer’s disease